
ABSTRACT:
In this article, we will discuss about the fascinating molecular and genetic basis of hepatitis. Hepatitis is a globally prevalent liver disease that affects millions of people each year. It is classified into several types, including hepatitis A, B, C, D, and E, all caused by different viruses. Understanding the molecular and genetic basis of hepatitis is crucial for developing effective treatments and preventive measures. In this article, we will delve into the intricate mechanisms and genetic factors that underlie this disease, using references to support our findings.
INTRODUCTION OF MOLECULAR AND GENETIC BASIS OF HEPATITIS:
Millions of individuals around the world are affected by hepatitis, a global health issue. It characterized by liver inflammation, which can result from a number of conditions, including viral infections, alcoholism, autoimmune illnesses, and exposure to specific chemicals. Hepatitis viruses A, B, C, D, and E are what cause viral hepatitis, the most prevalent type of hepatitis. For the creation of efficient diagnostic tools, therapeutic interventions, and preventative measures, it is essential to comprehend the molecular and genetic underpinnings of hepatitis.
TYPES OF HEPATITIS:
1. HEPATITIS A:
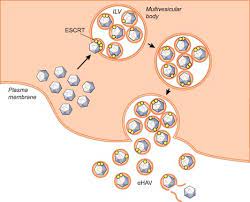
The main ways that the Hepatitis A virus (HAV) is spread through tainted food and water. It is an RNA virus that reproduces in liver cells and damages the liver by inducing inflammation. The genetic diversity of HAV strains shows ongoing virus evolution, which presents difficulties for the creation of vaccines.
2. HEPATITIS B:
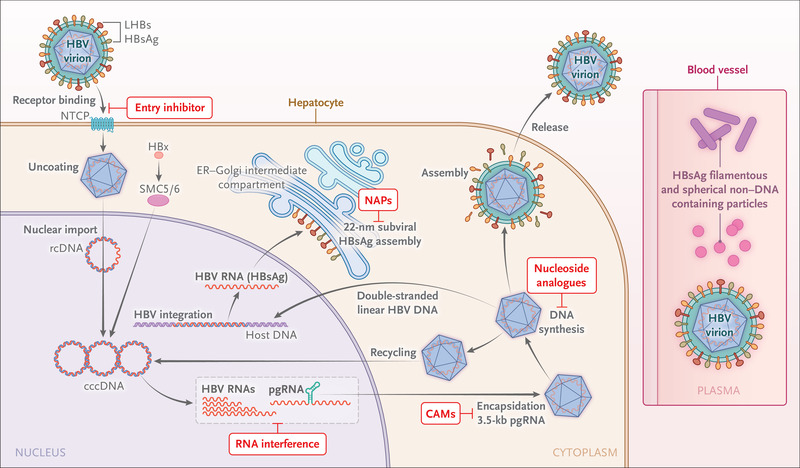
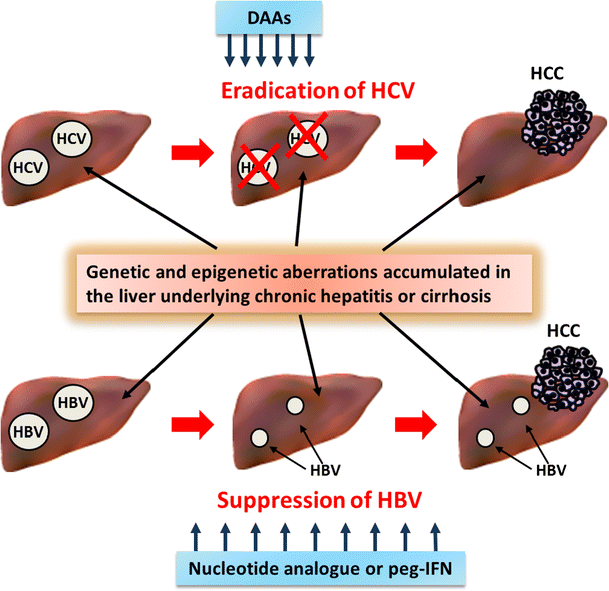
The partly double-stranded DNA virus known as the hepatitis B virus (HBV) can infect liver cells on a long-term basis. As the viral genome combines with the host DNA, a prolonged infection and an elevated risk of liver cancer result. The development of chronic hepatitis B is influenced on the basis the interaction of viral and host variables.
3. HEPATITIS C:
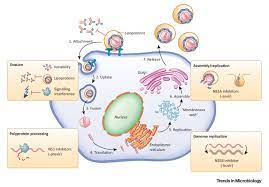
Hepatitis C virus (HCV) is an RNA virus that exhibits high genomic variability. The virus hijacks host cell machinery to replicate, leading to chronic infection in most cases. The genetic variability of HCV strains influences disease progression, treatment response, and vaccine development. Host genetic factors such as interleukin-28B polymorphisms also contribute to HCV infection outcomes.
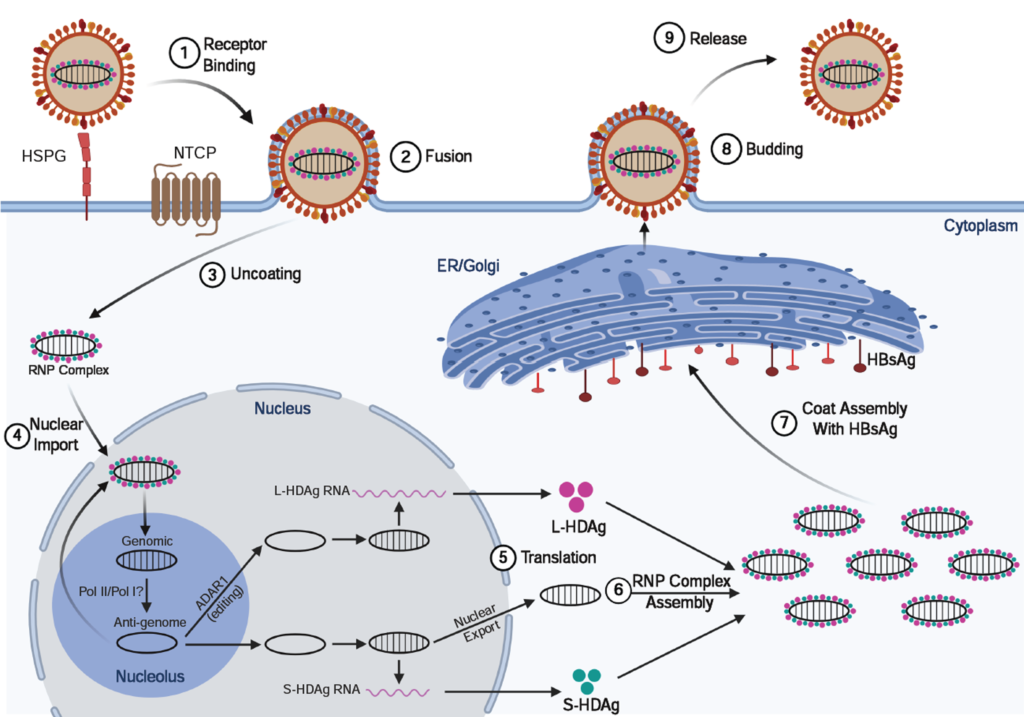
4. HEPATITIS D:
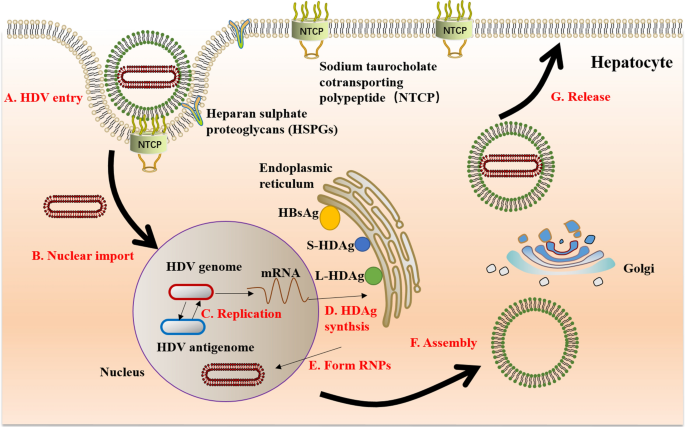
Hepatitis D, or delta hepatitis, is caused by the hepatitis D virus (HDV). HDV can only replicate in the presence of HBV, leading to superinfection or co-infection. HDV utilizes a ribozyme to replicate its RNA genome, which contributes to its unique life cycle and pathogenicity.
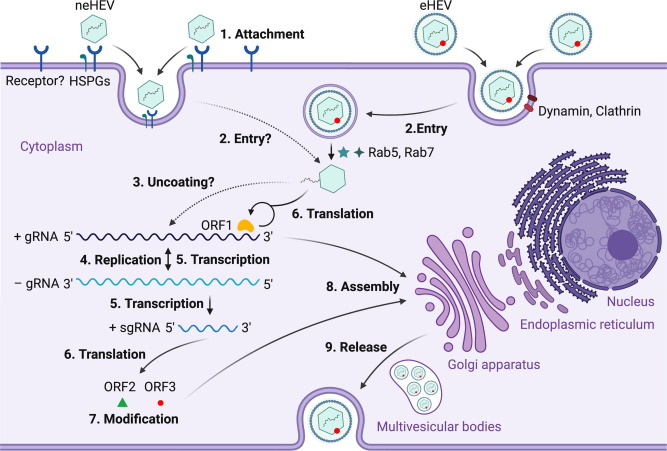
5. HEPATITIS E:
Hepatitis E virus (HEV) is a single-stranded RNA virus primarily transmitted through contaminated water. Although most cases of hepatitis E are acute and self-limiting, some individuals, especially pregnant women and individuals with compromised immune systems, may develop chronic infection. Genetic factors, including host immune responses, influence disease severity and progression.
MOLECULAR AND GENETIC BASIS OF HEPATITIS:
1. MOLECULAR BASIS OF HEPATITIS:
The interplay of the host immune system and the hepatitis virus forms the molecular basis of the disease. Hepatocytes, the primary functioning cells of the liver, are the primary target of hepatitis viruses, which are tiny, encapsulated viruses. After becoming infected, the virus replicates inside the hepatocytes, causing the release of viral particles and subsequent inflammation. In order to create viral proteins and replicate the viral genome, viruses hijack host cellular machinery, such as the transcription and translation machinery.
2. GENETIC BASIS OF HEPATITIS:
Genetic factors play a significant role in determining the susceptibility, progression, and outcome of hepatitis infections. Host genetic variations can influence the immune response to viral infections, viral clearance, and the development of chronic hepatitis. Several genes involved in the immune response, such as human leukocyte antigen (HLA) genes, cytokines, and interferon-stimulated genes, have implicated in the genetic basis of hepatitis. For example, certain HLA alleles have associated with increased susceptibility to hepatitis B and C viruses, while others have linked to better viral clearance.
CONCLUSION:
The molecular and genetic basis of hepatitis reveals the complex interplay between viral and host factors that contribute to disease progression, chronicity, and treatment response. Understanding these mechanisms is crucial for developing effective therapies and preventive strategies. Continued research on the molecular and genetic aspects of hepatitis will pave the way for novel diagnostic tools, vaccines, and targeted therapies in the fight against this global health burden. Recent studies have shed light on the role of host genetic factors, such as HLA genes and cytokines, in determining the susceptibility and outcome of hepatitis infections. Further research in this field will contribute to the development of personalized medicine approaches and targeted therapies for hepatitis patients.
REFERENCES:
Thio CL, Thomas DL, Goedert JJ, et al. Racial differences in HLA class II associations with hepatitis B virus outcomes. J Infect Dis. 2001;183(7):1138-1141. doi:10.1086/319277
Prokunina-Olsson L, Muchmore B, Tang W, et al. A variant upstream of IFNL3 (IL28B) creating a new interferon gene IFNL4 associated with impaired clearance of hepatitis C virus. Nat Genet. 2013;45(2):164-171. doi:10.1038/ng.2521 https://pubmed.ncbi.nlm.nih.gov/23291588/
Lemon SM, Ott JJ, Van Damme P, et al. Type A viral hepatitis: A summary and update on the molecular virology, epidemiology, pathogenesis and prevention. J Hepatol. 2017;68(1):167-184. https://pubmed.ncbi.nlm.nih.gov/28887164/
Kidd-Ljunggren K, Kidd AH. Genetic variability in hepatitis B viruses. J Gen Virol. 2011; 82(Pt 4): 859-880. https://pubmed.ncbi.nlm.nih.gov/12029141/
Li H, Zhang L. Genetic diversity of hepatitis C virus: Implications for pathogenesis, treatment and vaccine development. Virol J. 2016;13:1-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4146759/
Debing, Y., Gisa, A., Dallmeier, K., et al. A mutation in the human management of hepatitis E virus avirulence factor enhances viral replication in macrophages and dendritic cells. J Virol. 2014; 88(5), 2330-2339. https://pubmed.ncbi.nlm.nih.gov/25181691/

